Coeliac disease is a common autoimmune enteropathy triggered by the ingestion of gluten.
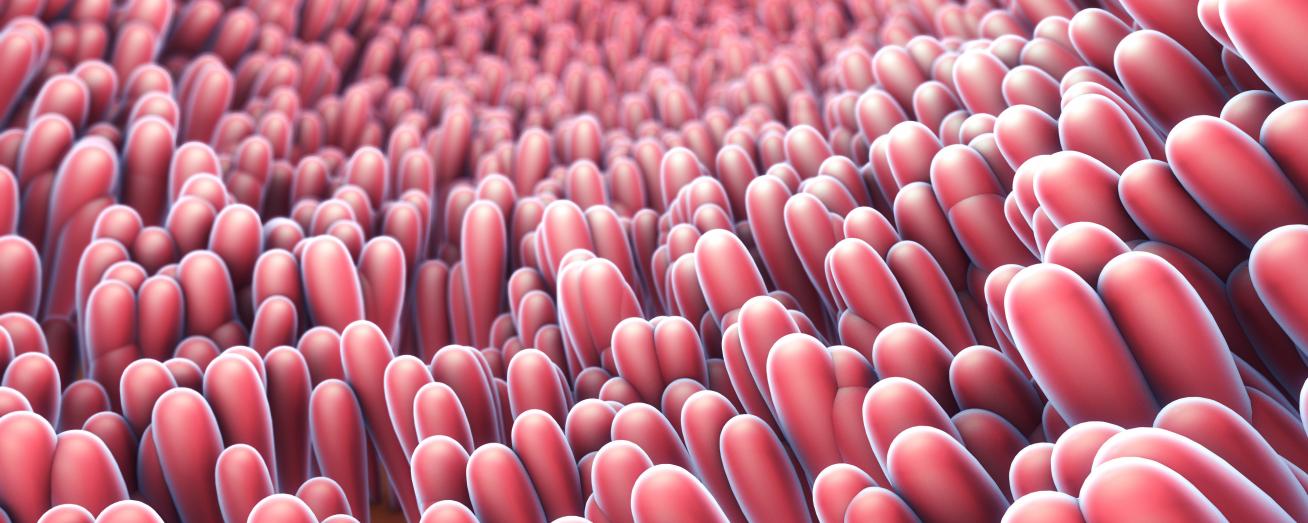
Coeliac disease is a permanent intolerance to gluten proteins found in a number of widely consumed cereal grains, including wheat, barley, spelt, rye, KAMUT®, and triticale. In children and adults with genetic predisposition, the ingestion of foods containing gluten causes an autoimmune reaction in the intestine. This results in chronic inflammation of the small intestinal mucosa and truncation of the villi, therefore reducing the absorptive capacity of the small intestine. If untreated, these characteristic histopathological changes result in malabsorption of key micronutrients and consequent nutritional deficiencies. However, the consumption of a strict gluten-free diet allows regeneration of the villi and resolution of symptoms. A lifelong gluten-free diet, in which all traces of gluten are avoided, is currently the only treatment available for the management of this condition.
Prevalence
Coeliac disease is more common than is often assumed. In the UK, 1 in 100 people are believed to have the condition, yet current research shows only 24% are actually diagnosed [1,2,3], largely due to the non-specific symptomatology often observed in presenting cases. Diagnosis rates are increasing, which appears to be a rise in incidence rather than awareness and detection [4].
In the UK, 1 in 100 people are believed to have the condition, yet current research shows only 24% are actually diagnosed.
Oslo definitions of coeliac disease
Due to lack of consensus on the use of terms related to coeliac disease and gluten, a multi-disciplinary task force of international physicians was convened to agree a set of definitions for the various types of coeliac disease based on presentation and symptoms, these were updated in 2013, and are referred to as ‘the Oslo definitions’ for coeliac disease and related terms [4]. The Oslo definitions are outlined below.
Classical coeliac disease
Coeliac disease presenting with signs and symptoms of malabsorption. Diarrhoea, steatorrhoea, weight loss or growth failure is required.
Non-classical coeliac disease
Coeliac disease presenting without signs and symptoms of malabsorption.
Subclinical coeliac disease
Coeliac disease that is below the threshold of clinical detection and without signs or symptoms sufficient to trigger coeliac testing in routine practice.
Symptomatic coeliac disease
Coeliac disease characterised by clinically evident gastrointestinal and/or extraintestinal symptoms attributable to gluten intake.
Potential coeliac disease
Individuals with a normal small intestinal mucosa who are at increased risk of developing coeliac disease as indicated by positive coeliac serology.
Refractory coeliac disease
Persistent or recurrent malabsorptive symptoms with villous atrophy despite a strict gluten free diet for more than 12 months.
Depending on the protein fraction, toxic peptides occur during degradation in the body, which lead to changes in the intestine of coeliac disease patients.

Reference
- West J, Logan RFA, Hill PG et al. Seroprevalence, correlates and characteristics of undetected coeliac disease in England. Gut 2003; 52:960-965
- Bingley PJ, Williams AJK, Norcross AJ et al. Undiagnosed coeliac disease at age seven: population-based prospective birth cohort study. BMJ 2004; 328:322-323
- West J, Fleming KM, Tata LJ et al. Incidence & Prevalence of celiac disease and dermatitis herpetiformis in the UK over two decades: Population-based study. American Journal of Gastroenterology 2014; 109:757-768.
- Lebwohl B, Sanders DS, Green PHR. Coeliac disease. Lancet 2018; 391: 70-81
- Ludvigsson JF, Leffler DA, Bai J. The Oslo definitions for coeliac disease and related terms. Gut 2013; 62:43-52.